Addressing Common Myths About Infiltration Needles
Infiltration Needles: Addressing Common Myths
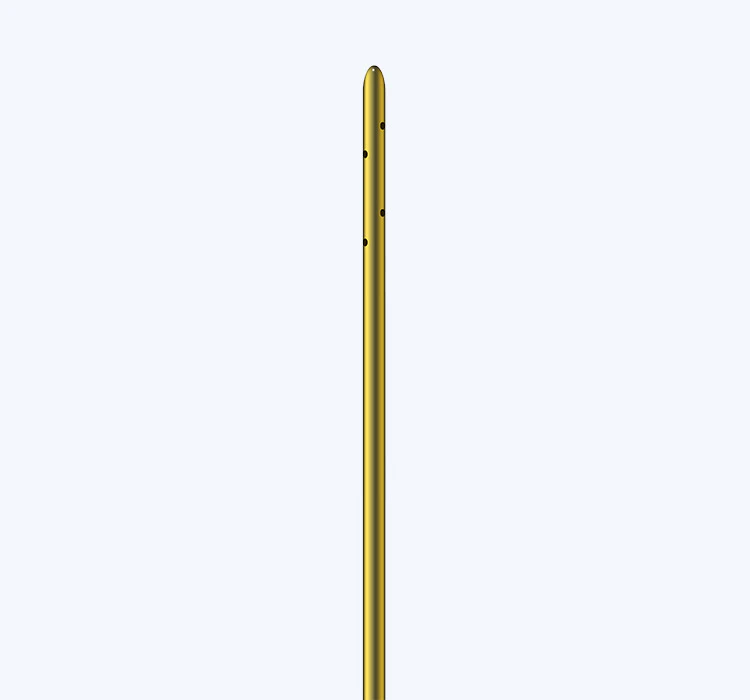
In the medical field, infiltration needles are a common tool used in a wide range of procedures. However, there are many myths and misconceptions surrounding these essential medical instruments. In this article, we will address some of the most common myths about infiltration needles and provide evidence-based information to set the record straight.
Myth: Infiltration needles are always painful
It's a common belief that infiltration needles are always associated with pain and discomfort for the patient. While it's true that some patients may experience discomfort during needle insertion, advances in needle design and the use of topical anesthetics have greatly reduced the level of pain associated with infiltration needle procedures. In fact, many patients report minimal discomfort during the use of infiltration needles, especially when a skilled medical professional is performing the procedure.
Infiltration needles are designed to deliver medication or fluids into the subcutaneous tissue, and modern needle technology has greatly improved the patient experience. For example, smaller-gauge needles are now available, which can reduce pain and tissue trauma. Additionally, the use of topical anesthetics can further minimize any discomfort associated with infiltration needle insertion. It's important for patients to communicate any concerns about pain with their healthcare provider, as there are often strategies that can be employed to mitigate discomfort during infiltration needle procedures.
Myth: Infiltration needles always cause bruising and tissue damage
Another common myth about infiltration needles is that they always cause bruising and tissue damage at the insertion site. While it's true that bruising and tissue damage can occur as a result of infiltration needle procedures, especially if the needle is inserted incorrectly or at too steep an angle, these issues are not inevitable. Skilled medical professionals are trained to minimize tissue trauma during infiltration needle procedures, and advances in needle technology have also contributed to reducing the risk of bruising and tissue damage.
One important consideration in minimizing tissue trauma is the selection of the appropriate needle gauge for the procedure. Smaller-gauge needles are associated with less tissue damage, as they create a smaller hole during insertion. Additionally, proper technique, including the use of a gentle, controlled approach to needle insertion, can also help to reduce the risk of bruising and tissue damage. It's important for healthcare providers to properly position the needle and advance it slowly and steadily to minimize trauma to the surrounding tissue.
Myth: Infiltration needles are always associated with infection risk
There is a pervasive myth that infiltration needles are always associated with a high risk of infection. While it's true that any invasive medical procedure carries some degree of infection risk, modern infiltration needles are designed with features that help to minimize this risk. For example, many infiltration needles are now equipped with safety mechanisms that reduce the likelihood of accidental needlesticks, which can help to prevent the transmission of infectious agents.
Proper sterilization and aseptic technique are also critical components of infection control during infiltration needle procedures. Healthcare providers are trained to adhere to strict protocols for hand hygiene, preparation of the skin at the insertion site, and the use of sterile gloves and equipment. These measures help to reduce the risk of introducing infectious agents during infiltration needle procedures.
It's important for patients to communicate any concerns about infection risk with their healthcare provider, as they can provide information about the specific infection control measures that will be used during the procedure. This can help to alleviate anxiety and provide reassurance about the safety of infiltration needle procedures.
Myth: Infiltration needles are always used for medication administration
While infiltration needles are commonly used for the administration of medications and fluids, there are also other applications for these versatile instruments. For example, infiltration needles are commonly used for the collection of blood samples for laboratory testing. In this context, the needle is inserted into a vein to obtain a blood sample, rather than into the subcutaneous tissue for medication administration.
Infiltration needles are also used for the delivery of local anesthetics prior to minor surgical procedures, such as the removal of skin lesions. The needle is used to introduce the anesthetic solution into the tissue surrounding the procedure site, providing effective pain management for the patient. By dispelling the myth that infiltration needles are exclusively used for medication administration, patients and healthcare providers can gain a better understanding of the wide range of clinical applications for these essential medical instruments.
Myth: Infiltration needles are always the best option for fluid administration
While infiltration needles are a valuable tool for the administration of medications and fluids, they are not always the best option in every clinical scenario. For example, in patients with compromised vascular access, such as those with fragile veins or a history of intravenous drug use, alternative methods of fluid administration may be more appropriate. In these cases, healthcare providers may choose to use specialized catheters or infusion devices to ensure safe and effective fluid delivery.
It's important for healthcare providers to carefully assess each patient's unique clinical situation and consider factors such as vascular integrity, fluid volume requirements, and the need for frequent blood sampling when determining the most appropriate method for fluid administration. By dispelling the myth that infiltration needles are always the best option for fluid administration, healthcare providers can ensure that patients receive the most appropriate and effective care for their individual needs.
In conclusion, there are many myths and misconceptions surrounding infiltration needles, and it's important to address these myths with evidence-based information. By dispelling common myths about pain, bruising, infection risk, clinical applications, and fluid administration, healthcare providers can effectively educate patients and promote understanding of the safe and effective use of infiltration needles in clinical practice. With the proper knowledge and understanding, patients and healthcare providers can work together to ensure the best possible outcomes for infiltration needle procedures.

 Español
Español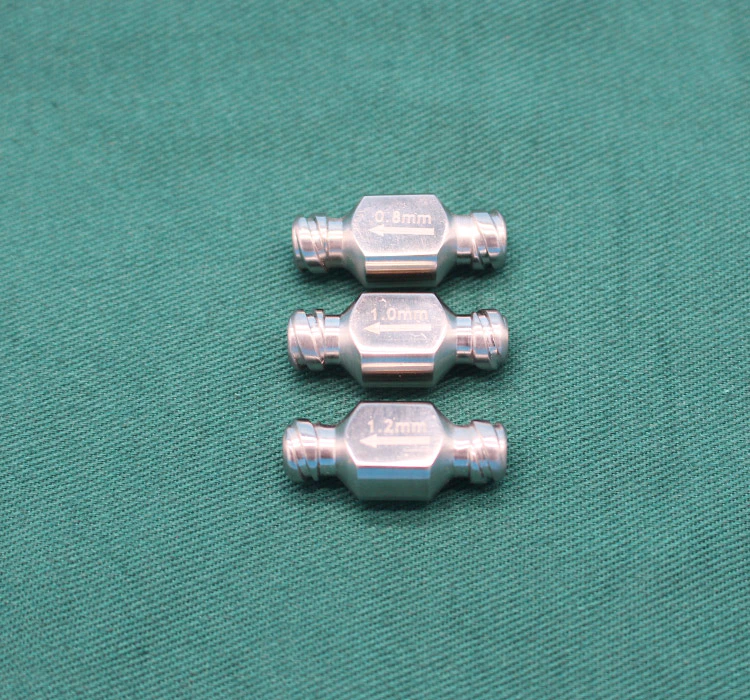



 Sales Manager : Kelly Zhou
Sales Manager : Kelly Zhou Email :
Email :  WhatsApp : +86 18067965386
WhatsApp : +86 18067965386