Best Practices for Using Infiltration Cannulas Effectively
Infiltration cannulas are commonly used in various medical procedures, including liposuction, tumescent anesthesia, and infiltration of drugs or fluids. To ensure the safe and effective use of infiltration cannulas, it is essential to follow best practices. In this article, we will explore the best practices for using infiltration cannulas effectively, including proper techniques, safety measures, and tips for maximizing the efficacy of the procedure.
Understanding the Basics of Infiltration Cannulas
Infiltration cannulas are specialized medical devices designed to deliver fluids, such as local anesthetic, saline solution, or medication, to targeted areas of the body. These cannulas typically consist of a hollow tube with a sharp, beveled tip that allows for precise insertion into the skin or tissue. Infiltration cannulas come in various sizes and configurations to accommodate different procedures and anatomical considerations.
When using infiltration cannulas, it is crucial to select the appropriate size and type for the specific procedure. Factors to consider include the volume of fluid to be delivered, the viscosity of the fluid, and the depth and location of the target tissue. Using the wrong size or type of cannula can lead to suboptimal results, increased risk of complications, and patient discomfort.
Proper training and education on the use of infiltration cannulas are essential for healthcare professionals to ensure safe and effective use. This includes understanding the anatomy of the target area, proper insertion techniques, and patient positioning to optimize access and visualization. Additionally, healthcare providers should be familiar with the indications for infiltration, potential contraindications, and strategies for minimizing patient discomfort during the procedure.
Best Practices for Sterilization and Aseptic Technique
Maintaining a sterile field and employing aseptic technique are critical when using infiltration cannulas to minimize the risk of infection and ensure patient safety. Before using a cannula, it must be properly sterilized according to industry standards and institutional protocols. This typically involves thorough cleaning, disinfection, and proper storage to prevent contamination.
Healthcare providers should also practice proper hand hygiene and wear appropriate personal protective equipment, such as gloves and gowns, when using infiltration cannulas. This helps prevent the introduction of microorganisms from the hands or clothing into the sterile field or the patient's tissues. Adhering to strict aseptic technique can reduce the risk of post-procedural complications, such as surgical site infections, and promote optimal healing.
In addition to maintaining a sterile environment during the procedure, it is essential to monitor the patient for signs of infection or adverse reactions following infiltration. This includes assessing for redness, swelling, warmth, or drainage at the cannula insertion site, as well as monitoring for systemic signs of infection, such as fever or malaise. Healthcare providers should educate patients on the signs and symptoms of infection and instruct them to seek immediate medical attention if any concerns arise.
Optimizing Fluid Delivery and Distribution
One of the key goals of using infiltration cannulas is to deliver fluids, such as local anesthetic or tumescent solution, to the target tissues in a controlled and uniform manner. To achieve this, healthcare providers must pay attention to several factors, including the rate of fluid delivery, the pressure applied during infiltration, and the distribution of the fluid within the tissues.
When using infiltration cannulas, it is crucial to maintain a steady and controlled rate of fluid delivery to avoid overloading the tissues or causing excessive swelling. This may involve adjusting the infusion rate based on the patient's response, the size of the treatment area, and the type of fluid being delivered. Providers should also be mindful of the pressure applied during infiltration to prevent tissue trauma or inadvertent intravascular injection.
In some cases, the use of specialized infiltration techniques, such as tumescent infiltration, may be necessary to achieve optimal fluid distribution within the target tissues. Tumescent infiltration involves the use of a large volume of dilute anesthetic solution to create tumescence or tissue swelling, which can facilitate the dissection of tissues, minimize bleeding, and enhance patient comfort during surgical procedures. Healthcare providers should be familiar with the principles and techniques of tumescent infiltration to maximize its benefits and minimize potential complications.
Minimizing Patient Discomfort and Complications
Infiltration cannulas are often used in procedures that involve the administration of local anesthesia or tumescent solution, which can cause discomfort or pain for the patient. To minimize patient discomfort, healthcare providers should consider using smaller gauge cannulas, employing slower infiltration rates, and using proper anesthesia techniques to ensure adequate pain control.
In addition to minimizing patient discomfort, it is important to monitor for potential complications associated with the use of infiltration cannulas, such as tissue trauma, hematoma formation, and inadvertent intravascular injection. Providers should be vigilant for signs of complications and be prepared to intervene as needed to mitigate their impact on the patient's outcome.
Furthermore, educating patients on what to expect during and after the procedure, including potential side effects and complications, can help manage their expectations and alleviate anxiety. Providing patients with clear instructions for post-procedural care and symptom management can contribute to a positive patient experience and improve overall satisfaction with the procedure.
Post-procedural Care and Follow-up Monitoring
After using infiltration cannulas, it is essential to provide comprehensive post-procedural care and monitoring to ensure optimal healing and patient safety. This may include applying appropriate dressings, providing pain management instructions, and giving patients specific guidelines for activity restrictions and wound care.
Healthcare providers should also schedule follow-up appointments to assess the patient's progress, monitor for any signs of infection or complications, and address any concerns or questions the patient may have. Follow-up monitoring can help ensure that the patient is healing as expected and can provide an opportunity to address any issues that may arise in a timely manner.
In some cases, patients who undergo procedures involving infiltration cannulas may require additional interventions or touch-up procedures to achieve the desired results. It is essential for healthcare providers to have open communication with patients and be prepared to offer additional support or follow-up care as needed to optimize the patient's outcomes and satisfaction.
In conclusion, using infiltration cannulas effectively requires attention to various factors, including proper technique, sterile practice, fluid delivery, patient comfort, and post-procedural care. Adhering to best practices when using infiltration cannulas can help minimize the risk of complications, optimize patient outcomes, and improve the overall quality of care provided. By staying informed about the latest developments and techniques in infiltration procedures, healthcare providers can continue to enhance their skills and deliver safe and effective care to their patients. Remember, the effective use of infiltration cannulas is crucial for achieving successful outcomes and ensuring patient satisfaction. With the right knowledge and training, healthcare providers can utilize infiltration cannulas with confidence and achieve optimal results for their patients.

 Español
Español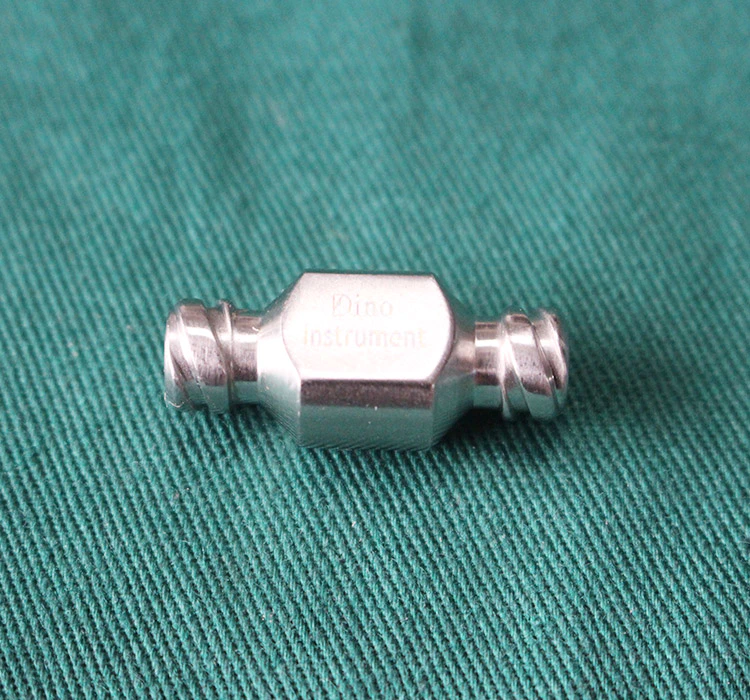




 Sales Manager : Kelly Zhou
Sales Manager : Kelly Zhou Email :
Email :  WhatsApp : +86 18067965386
WhatsApp : +86 18067965386