Infiltration Cannulas in Dermatology: Effective Pain Control
Infiltration Cannulas in Dermatology: Effective Pain Control
Introduction:
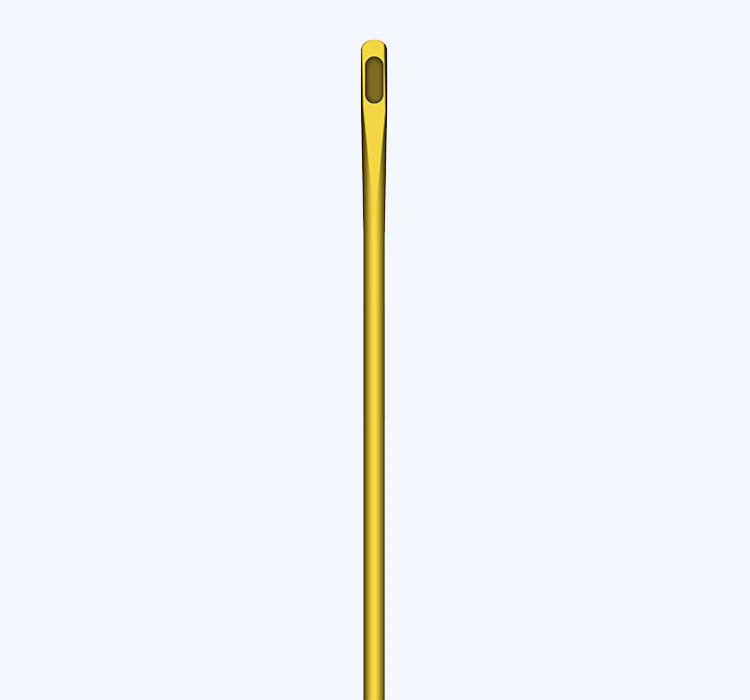
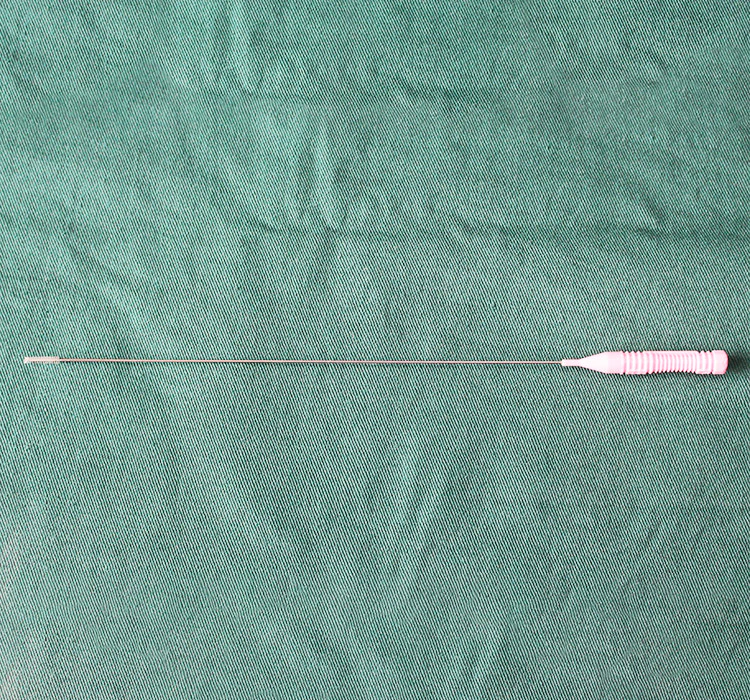
In the field of dermatology, pain control during various procedures is of paramount importance for both the patient's comfort and successful outcomes. One promising solution that has gained popularity is the use of infiltration cannulas. These specialized instruments allow for the targeted delivery of local anesthetics, providing effective pain relief during dermatological procedures. This article explores the diverse applications, advantages, limitations, and future prospects of infiltration cannulas in the realm of dermatology.
Advancing Dermatological Procedures with Infiltration Cannulas:
1. Anesthetic Administration for Biopsies and Excisions:
Dermatological procedures such as skin biopsies and excisions often involve local anesthesia to ensure the patient's comfort. Infiltration cannulas are skillfully employed by dermatologists to deliver a precise dose of anesthetic directly into the target area. The cannula's thin, sharp tip, accompanied by its robust design, ensures accurate placement and controlled administration of anesthesia.
2. Utilizing Infiltration Cannulas for Laser Treatments:
Laser treatments are widely used in dermatology for various purposes, including hair removal, tattoo removal, and skin rejuvenation. These procedures can be uncomfortable and mildly painful for patients. Infiltration cannulas, when combined with local anesthetics, provide effective pain control without compromising the laser's efficacy. By infiltrating the anesthetic in the targeted area, dermatologists can perform laser procedures more comfortably and accurately.
3. Enhancing Patient Comfort during Dermal Filler Injections:
Dermal fillers are commonly used to restore volume, reduce wrinkles, and enhance facial features. However, these injections can lead to discomfort, especially in sensitive areas. Infiltration cannulas offer an innovative approach to mitigate pain during dermal filler injections. Dermatologists can infiltrate a small anesthetic solution in the treatment area using cannulas, allowing for painless, precise, and controlled filler administration.
4. Addressing Pain During Aesthetic Dermatology Procedures:
Aesthetic dermatology procedures, such as chemical peels and micro-needling, can cause considerable discomfort. Infiltration cannulas have emerged as a valuable tool to alleviate this pain by administering local anesthetics subcutaneously. By employing cannulas, dermatologists can perform aesthetic procedures more comfortably, leading to increased patient satisfaction and adherence to treatment plans.
5. Comprehensive Pain Control in Mohs Surgery:
Mohs surgery is a precise technique used to remove skin cancers while minimizing damage to surrounding healthy tissue. This procedure can be lengthy, intricate, and often accompanied by discomfort. Infiltration cannulas play a crucial role in this surgical method by providing localized pain relief throughout the stages of tumor removal. Dermatologists can skillfully infiltrate anesthetic solutions into the surgical site using cannulas, ensuring patient comfort without compromising the surgery's precision.
Advantages, Limitations, and Future Prospects:
Infiltration cannulas offer several advantages over traditional pain control methods in dermatology. Firstly, they allow for precise and targeted administration of anesthetic solutions, reducing unnecessary exposure to unaffected areas. Secondly, the use of cannulas minimizes the risks associated with surface anesthesia techniques, such as contact dermatitis or systemic toxicity. Moreover, infiltration cannulas are easy to use, economical, and compatible with various anesthetic agents.
However, it is vital to acknowledge the limitations of infiltration cannulas. The cannulas require technical proficiency, and their use may necessitate additional time during procedures. Furthermore, there is a potential risk of hematoma formation or inadvertent damage to blood vessels, highlighting the importance of dermatologists' experience and expertise in the field. Despite these limitations, ongoing research and technological advancements are expected to address and improve upon these challenges.
The future of infiltration cannulas in dermatology appears promising. Advancements in cannula design and needle manufacturing have led to the development of ultra-thin, flexible, and atraumatic cannulas, further enhancing patient comfort and safety. Additionally, researchers are actively exploring novel anesthetic formulations and delivery methods to optimize pain control during dermatological procedures. Continuous innovation and collaboration between dermatologists and medical device manufacturers will undoubtedly contribute to the wider adoption and advancement of infiltration cannulas in pain control within the field of dermatology.
Conclusion:
Infiltration cannulas have proven to be an effective tool for pain control in dermatological procedures. Their precise delivery of local anesthetics ensures patients' comfort, enhances procedural accuracy, and leads to better treatment outcomes. By employing infiltration cannulas, dermatologists can offer painless and efficient solutions in various dermatology subspecialties, including biopsies, laser treatments, dermal filler injections, aesthetic procedures, and Mohs surgery. Continued research and technological advancements will further improve the safety, efficacy, and versatility of infiltration cannulas, reinforcing their significance in modern dermatological practice.

 Español
Español


 Sales Manager : Kelly Zhou
Sales Manager : Kelly Zhou Email :
Email :  WhatsApp : +86 18067965386
WhatsApp : +86 18067965386