Patient Education: What to Expect with Infiltration Cannulas
Infiltration cannulas are medical devices used in a variety of clinical settings. These cannulas are designed to deliver medication, fluids, or other types of solutions directly into the body's tissues. Whether you are a patient receiving treatment through infiltration cannulas or a healthcare professional administering them, it is important to understand what to expect during the process.
Understanding Infiltration Cannulas
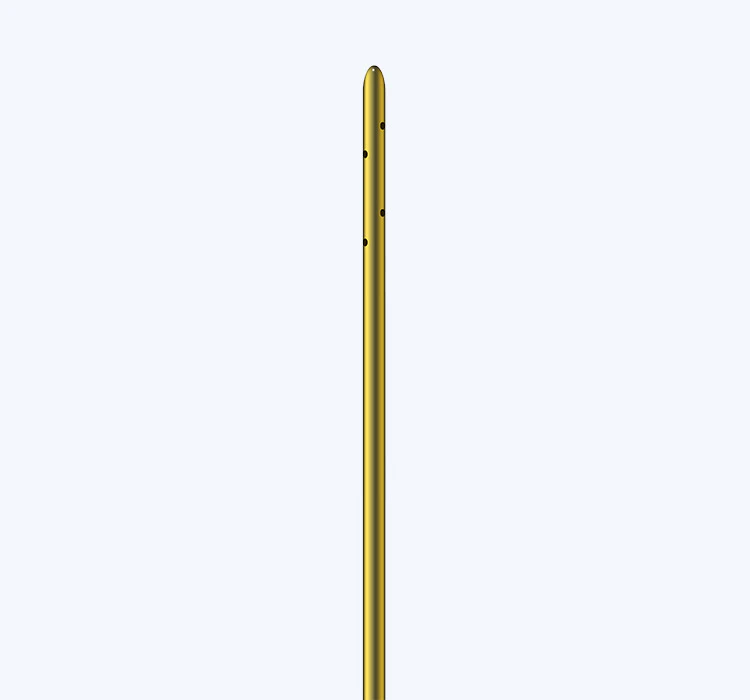
Infiltration cannulas, also known as winged infusion sets or scalp vein sets, are small, flexible tubes with a needle at one end and a connector for tubing at the other. The needle end is inserted into the patient's vein, while the tubing end is attached to a syringe or IV line for the delivery of fluids or medications. These devices are commonly used in situations where direct access to a vein is required, such as during blood draws, intravenous drug administration, or IV fluid therapy.
When using infiltration cannulas, healthcare providers carefully select an appropriate size and gauge based on the patient's age, weight, and clinical needs. The choice of cannula size and gauge is crucial to ensuring safe and effective delivery of fluids or medications while minimizing the risk of complications such as infiltration, which occurs when the solution leaks into the surrounding tissue instead of entering the vein.
Uses of Infiltration Cannulas
Infiltration cannulas serve a variety of purposes in clinical practice. One common use is for blood draws, where the cannula is inserted into a vein to collect a sample for laboratory testing. Additionally, infiltration cannulas are frequently utilized for intravenous (IV) therapy, in which fluids, electrolytes, medications, or blood products are administered directly into the bloodstream to treat dehydration, nutritional deficiencies, infections, or other medical conditions.
In pediatric care, infiltration cannulas are often preferred over traditional needles for venipuncture and IV access, as they provide a more secure and stable connection while minimizing patient discomfort. Moreover, infiltration cannulas are frequently employed for the administration of contrast agents during diagnostic imaging procedures such as computed tomography (CT) scans and magnetic resonance imaging (MRI) studies.
In outpatient settings, infiltration cannulas are used for procedures such as chemotherapy, blood transfusions, and intravenous infusions of antibiotics or other medications. The versatility of infiltration cannulas makes them indispensable tools for healthcare professionals across various specialties, including emergency medicine, critical care, oncology, and pediatrics.
Placement and Insertion Techniques
Proper placement and insertion of infiltration cannulas are essential for ensuring patient safety and comfort. Healthcare providers must follow established protocols for venipuncture and cannula insertion, which require meticulous attention to detail and adherence to aseptic techniques to prevent infection.
Before inserting the cannula, the healthcare provider assesses the patient's veins to identify the most suitable site for access. Factors such as vein size, visibility, and accessibility are taken into consideration when choosing the insertion site. For pediatric patients or individuals with difficult venous access, the use of techniques such as transillumination or ultrasound guidance may be beneficial in locating suitable veins for cannulation.
Once the insertion site is identified, the healthcare provider prepares the area by cleaning the skin with an antiseptic solution to minimize the risk of contamination. The cannula is then inserted into the vein at a slight angle, and the needle is gently advanced until blood return is observed, indicating successful venipuncture. Following confirmation of blood return, the needle is partially withdrawn, and the cannula is advanced into the vein while ensuring that the wings or adhesive base are securely anchored to the skin.
After securing the cannula in place, the healthcare provider connects the tubing to the appropriate administration set, such as a syringe or IV line, and begins the infusion of fluids or medications. Throughout the procedure, the healthcare provider monitors the cannula site for signs of infiltration, such as swelling, pain, or blanching of the surrounding tissue, and takes prompt action to address any complications that may arise.
Care and Maintenance of Infiltration Cannulas
Proper care and maintenance of infiltration cannulas are crucial to prevent complications and ensure their safe and effective use. After insertion, the healthcare provider secures the cannula with a transparent dressing or an adhesive bandage to protect the site and provide stability. It is essential to regularly assess the cannula site for signs of infiltration, infection, or dislodgement and to document these observations in the patient's medical record.
Patients receiving treatment through infiltration cannulas are educated on how to care for the site and are instructed to report any discomfort, pain, or changes in the appearance of the surrounding tissue to their healthcare provider immediately. Additionally, patients are advised to avoid excessive movement or trauma to the cannula site to minimize the risk of complications.
Healthcare providers must adhere to aseptic techniques when accessing and administering fluids or medications through infiltration cannulas to prevent infection and contamination. This includes using sterile gloves, cleaning the injection port with an antiseptic swab before each use, and replacing the cannula and tubing according to the manufacturer's recommendations or institutional policies.
Furthermore, routine assessment of the patency and integrity of infiltration cannulas is essential to ensure their proper function. Healthcare providers routinely inspect the cannula site for signs of blood return, kinking of the tubing, or other issues that may impede the flow of fluids or medications. Should any concerns arise, the healthcare provider takes appropriate action to address the problem and maintain the integrity of the cannula and its associated equipment.
Patient Education and Communication
Effective patient education and communication are integral to ensuring optimal outcomes with infiltration cannulas. Healthcare providers must take the time to educate patients and their caregivers on the purpose of infiltration cannulas, the procedural steps involved, and the potential benefits and risks associated with their use. Patients should be encouraged to ask questions and seek clarification on any aspects of their treatment involving infiltration cannulas to alleviate anxiety and promote active participation in their care.
In addition to verbal instruction, written materials and visual aids may be utilized to reinforce key concepts and provide patients with a reference for self-care at home. Patients should be informed about the signs and symptoms of infiltration, such as swelling, pain, or the absence of blood return, and instructed on when to seek medical attention if these issues arise.
Furthermore, open and transparent communication between healthcare providers and patients is essential for building trust and rapport. Patients should feel empowered to express their concerns, preferences, and any discomfort or anxiety they may experience during the use of infiltration cannulas. By fostering a collaborative and patient-centered approach, healthcare providers can enhance the overall experience for patients receiving treatment through infiltration cannulas and mitigate potential challenges associated with their use.
In summary, infiltration cannulas are indispensable tools in modern healthcare, facilitating the safe and effective delivery of fluids, medications, and other solutions to patients in diverse clinical settings. Understanding the uses, insertion techniques, care and maintenance, and patient education associated with infiltration cannulas is essential for healthcare professionals and patients alike. By prioritizing patient safety, communication, and adherence to best practices, healthcare providers can optimize the utilization of infiltration cannulas and promote positive outcomes for those under their care.

 Español
Español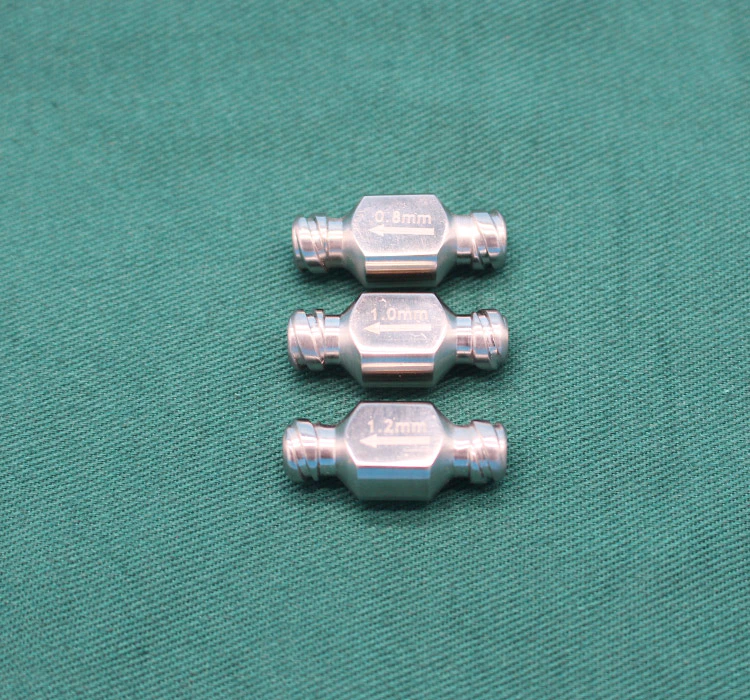



 Sales Manager : Kelly Zhou
Sales Manager : Kelly Zhou Email :
Email :  WhatsApp : +86 18067965386
WhatsApp : +86 18067965386