Safety Protocols for Infiltration Cannula Use in Procedures
Infiltration cannulas are commonly used in various medical procedures, including liposuction, fat transfer, and other aesthetic treatments. However, the use of infiltration cannulas comes with certain risks, and it is important to follow safety protocols to ensure the well-being of both the patient and the medical staff involved in the procedure. In this article, we will discuss the various safety protocols that should be followed when using infiltration cannulas in medical procedures.
Understanding the Risks of Infiltration Cannula Use
Infiltration cannulas are used to deliver fluids, such as tumescent solution or local anesthetic, to the treatment area during various medical procedures. While they are essential for these procedures, the use of infiltration cannulas carries certain risks, including the potential for tissue damage, fluid overload, and infection. It is crucial for medical professionals to understand these risks and take appropriate measures to minimize them.
When using infiltration cannulas, one of the main concerns is the potential for tissue damage. The sharp tip of the cannula can cause trauma to the surrounding tissue if not handled with care. Additionally, the pressure exerted by the fluid being delivered through the cannula can also contribute to tissue damage if proper technique is not followed. To minimize the risk of tissue damage, medical practitioners should undergo thorough training on the proper use of infiltration cannulas and ensure that they are using the appropriate cannula size and type for the specific procedure.
Another significant risk associated with infiltration cannula use is fluid overload, which occurs when an excessive amount of fluid is delivered to the treatment area. This can lead to complications such as pulmonary edema, electrolyte imbalance, and cardiovascular issues. To prevent fluid overload, it is important to calculate the maximum safe dose of tumescent solution or local anesthetic based on the patient's weight and overall health status. Additionally, monitoring the patient's vitals throughout the procedure can help identify any signs of fluid overload early on.
Infection is also a concern when using infiltration cannulas, as the introduction of the cannula into the body creates a potential pathway for pathogens to enter. To reduce the risk of infection, medical practitioners should adhere to strict aseptic techniques, including proper hand hygiene, sterilization of equipment, and the use of sterile drapes and gloves during the procedure. Additionally, using single-use, disposable cannulas can help minimize the risk of cross-contamination and infection.
Implementing Safety Protocols for Infiltration Cannula Use
To ensure the safe and effective use of infiltration cannulas in medical procedures, it is essential to implement specific safety protocols. These protocols should outline the steps to be followed before, during, and after the procedure to minimize the risks associated with infiltration cannula use.
Before the procedure, it is crucial to conduct a thorough patient assessment to identify any underlying medical conditions or contraindications that may increase the risks associated with infiltration cannula use. This assessment should include a review of the patient's medical history, current medications, and any known allergies. Additionally, obtaining informed consent from the patient and discussing the potential risks and benefits of the procedure is essential to ensure that the patient is fully aware of what to expect.
During the procedure, it is important to use the appropriate infiltration cannula size and type for the specific treatment area and the volume of fluid to be delivered. The use of blunt-tipped cannulas can help minimize the risk of tissue damage, particularly in sensitive areas such as the face or neck. Medical practitioners should also be trained in the proper technique for using infiltration cannulas, including the angle of insertion, depth of penetration, and the rate of fluid delivery. This training should be reinforced through regular skills assessments and continuing education.
After the procedure, it is important to monitor the patient closely for any signs of complications, such as excessive swelling, pain, or changes in vital signs. Providing clear post-procedure instructions to the patient, including information on potential side effects and when to seek medical attention, can help ensure a smooth recovery process. Additionally, documenting the details of the procedure, including the type and volume of fluid used, the specific cannula size and type, and any complications that arise, is essential for quality assurance and risk management purposes.
Ensuring Patient Safety and Comfort
In addition to following safety protocols for infiltration cannula use, it is important to prioritize patient safety and comfort throughout the entire procedure. Patients should be adequately informed about the procedure and prepared for what to expect during and after the treatment. This includes discussing any potential side effects or discomfort that may occur during the delivery of the tumescent solution or local anesthetic.
To ensure patient comfort during the procedure, medical practitioners should use appropriate techniques for pain management, such as the use of topical or local anesthetics before the insertion of the infiltration cannula. Additionally, maintaining open communication with the patient throughout the procedure can help alleviate any anxiety or discomfort they may experience.
After the procedure, patients should receive clear instructions on how to care for the treated area and manage any discomfort or swelling that may occur. Providing follow-up care and monitoring the patient's progress in the days and weeks following the procedure is essential to ensure a positive treatment outcome and address any concerns that may arise.
Adhering to Regulatory Guidelines and Standards
In addition to implementing safety protocols for infiltration cannula use, medical practitioners must also adhere to regulatory guidelines and standards set forth by relevant governing bodies. This includes ensuring compliance with licensing, credentialing, and scope of practice requirements for the use of infiltration cannulas in medical procedures.
For example, in the United States, the use of infiltration cannulas in procedures such as liposuction is regulated by organizations such as the American Society of Plastic Surgeons (ASPS) and the American Association for Accreditation of Ambulatory Surgery Facilities (AAAASF). These organizations have established specific guidelines and standards for the safe and effective use of infiltration cannulas, and medical practitioners must adhere to these requirements to maintain their accreditation and ensure patient safety.
Medical practitioners should also stay informed about any updates or changes to regulatory guidelines and standards related to infiltration cannula use, as these may impact their practice and the protocols they are required to follow. Regular training and education on regulatory compliance can help ensure that medical practitioners are up to date on the latest requirements and best practices for the use of infiltration cannulas in procedures.
Conclusion
In conclusion, the use of infiltration cannulas in medical procedures comes with certain risks, including tissue damage, fluid overload, and infection. To ensure the safe and effective use of infiltration cannulas, it is essential to implement specific safety protocols that address these risks. This includes conducting thorough patient assessments, using the appropriate cannula size and type, adhering to aseptic techniques, and monitoring patients for any signs of complications. Additionally, prioritizing patient safety and comfort, and adhering to regulatory guidelines and standards, is crucial for mitigating the risks associated with infiltration cannula use. By following these safety protocols, medical practitioners can help ensure the well-being of both the patient and the medical staff involved in the procedure.

 Español
Español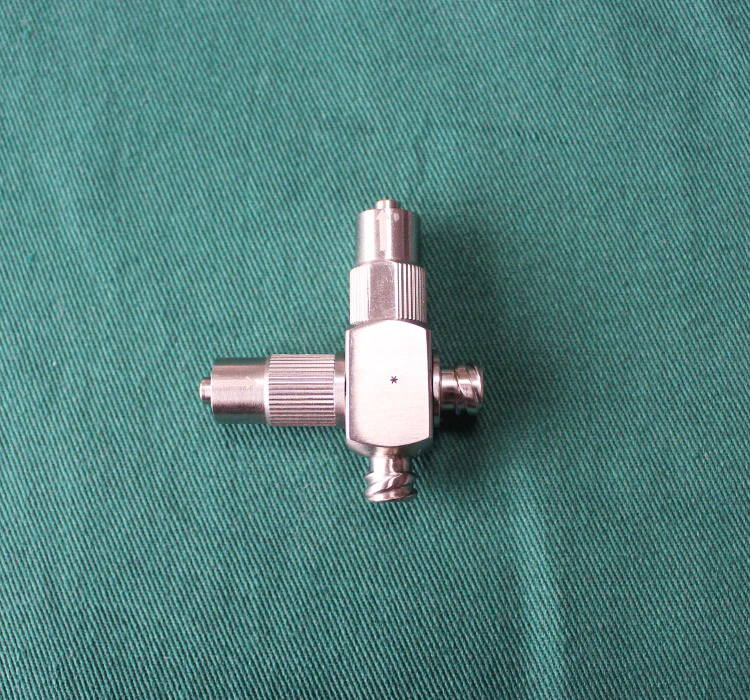




 Sales Manager : Kelly Zhou
Sales Manager : Kelly Zhou Email :
Email :  WhatsApp : +86 18067965386
WhatsApp : +86 18067965386